The Unmet Need: Why Traditional Cancer Therapies Fall Short
For decades, the battle against cancer has relied heavily on conventional methods such as chemotherapy, radiation therapy, and surgery. While these approaches have saved countless lives, they often come with significant drawbacks. Chemotherapy, for instance, operates with a broad stroke, attacking rapidly dividing cells—both cancerous and healthy—leading to severe side effects like hair loss, nausea, fatigue, and compromised immune systems. Similarly, radiation therapy, while more localized, can still damage surrounding healthy tissues. The fundamental challenge lies in achieving specificity: how to deliver potent therapeutic agents precisely to malignant cells while sparing healthy ones. This critical unmet need in cancer treatment has spurred intense cancer research into more sophisticated, targeted approaches, with nanotechnology emerging as a beacon of hope.
Nanotechnology: A Paradigm Shift in Oncology
Nanotechnology involves the manipulation of matter on an atomic, molecular, and supramolecular scale, typically ranging from 1 to 100 nanometers. At this minuscule dimension, materials exhibit unique physical, chemical, and biological properties that differ significantly from their bulk counterparts. These novel properties make nanomaterials exceptionally well-suited for biomedical applications, particularly in oncology. By designing nanoparticles with specific characteristics, scientists can overcome many limitations of traditional therapies, ushering in an era of precision medicine for cancer.
The Core Principle: Targeted Drug Delivery
The cornerstone of nanomedicine in cancer is targeted drug delivery. Instead of flooding the entire body with toxic drugs, nanoparticles can be engineered to concentrate therapeutic agents specifically at tumor sites. This targeting can occur through two primary mechanisms:
- Passive Targeting (EPR Effect): Tumor tissues often have leaky vasculature and impaired lymphatic drainage, leading to an "Enhanced Permeability and Retention" (EPR) effect. Nanoparticles, due to their size, can extravasate through these leaky vessels and accumulate within the tumor microenvironment, where they are retained for longer periods. This inherent biological phenomenon allows for passive accumulation of nanomedicines.
- Active Targeting: For even greater specificity, nanoparticles can be functionalized with targeting ligands on their surface. These ligands (e.g., antibodies, peptides, aptamers, or small molecules) specifically bind to receptors or antigens overexpressed on the surface of cancer cells. This lock-and-key mechanism ensures that the drug-loaded nanoparticles are actively taken up by the malignant cells, maximizing therapeutic efficacy while minimizing off-target effects on healthy tissues. This precise approach is central to advancing cancer treatment.
Diverse Nanocarriers: Tailoring Solutions for Cancer
The versatility of nanotechnology is evident in the wide array of nanocarriers developed for targeted drug delivery. Each type offers unique advantages, making them suitable for different therapeutic strategies in oncology:
- Liposomes: These spherical vesicles made of lipid bilayers are among the most clinically advanced nanocarriers, with several FDA-approved formulations. They can encapsulate both hydrophilic and hydrophobic drugs and offer good biocompatibility.
- Polymeric Nanoparticles: Biodegradable polymers can be engineered to form nanoparticles that encapsulate drugs, providing controlled and sustained release. Their customizable nature allows for fine-tuning of drug release kinetics and targeting capabilities.
- Dendrimers: Highly branched, tree-like macromolecules with precise, symmetrical structures. Their numerous surface groups allow for high drug loading capacity and multi-functionalization, making them excellent candidates for complex drug delivery systems in cancer research.
- Inorganic Nanoparticles: Materials like gold nanoparticles, magnetic nanoparticles, and quantum dots are being explored for their unique optical, magnetic, and thermal properties. Gold nanoparticles, for instance, can be used for photothermal therapy, where they convert light into heat to ablate tumor cells, or for enhanced imaging.
Beyond Delivery: Nanotechnology in Diagnostics and Synergistic Therapies
The impact of nanotechnology extends far beyond just drug delivery. It is profoundly transforming cancer diagnostics and enabling synergistic therapeutic approaches:
Revolutionizing Cancer Diagnostics and Imaging
Nanomaterials offer unprecedented sensitivity and specificity for early cancer detection and precise imaging. Nanobiosensors can detect minute quantities of biomarkers in blood or urine, facilitating early diagnosis even before symptoms appear. Quantum dots and other fluorescent nanoparticles provide superior contrast agents for medical imaging, allowing for clearer visualization of tumors and metastases, and enabling real-time monitoring of treatment response. This advancement is crucial for improving patient outcomes in oncology.
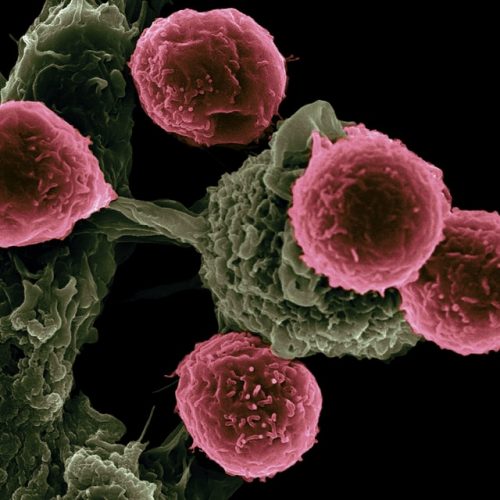
Synergistic Approaches: Nanotechnology with Gene and Immunotherapy
The true power of nanotechnology lies in its ability to integrate with and amplify other cutting-edge therapies. In gene therapy, nanoparticles serve as efficient, non-viral vectors for delivering therapeutic nucleic acids (like siRNA, miRNA, or CRISPR components) directly into cancer cells, modulating gene expression to inhibit tumor growth or sensitize cells to chemotherapy. This intersection with molecular biology is opening new frontiers.
Furthermore, nanotechnology is playing a pivotal role in advancing immunotherapy. Nanoparticles can encapsulate and deliver immunomodulators, vaccines, or checkpoint inhibitors directly to immune cells within the tumor microenvironment, enhancing the body's natural anti-cancer response. This targeted approach minimizes systemic side effects often associated with traditional immunotherapies, making them more effective and tolerable for patients. The synergy between biotechnology and nanotechnology promises a future of highly personalized and potent cancer treatments.
Challenges and the Bright Future of Nano-Oncology
Despite the immense promise, the journey of nanotechnology from lab to clinic faces several hurdles. Challenges include ensuring the long-term safety and biocompatibility of nanoparticles, scaling up their production for clinical use, and navigating complex regulatory pathways. However, ongoing cancer research is steadily addressing these issues, with significant progress in understanding nanoparticle interactions with biological systems and developing robust manufacturing processes.
The future of nano-oncology is incredibly bright. We can anticipate the development of "smart" nanoparticles that respond to specific tumor microenvironment cues (e.g., pH, enzyme levels) to release drugs precisely when and where needed. Personalized nanomedicine, tailored to an individual patient's genetic profile and tumor characteristics, will become increasingly prevalent. The integration of artificial intelligence and machine learning will further accelerate the design and optimization of novel nanocarriers, pushing the boundaries of what's possible in cancer treatment.
Advance Your Expertise with Deep Science Workshops & Deep Science Implementation
The rapid evolution of nanotechnology in cancer research demands a new generation of skilled professionals. At Deep Science Workshops and Deep Science Implementation, we are committed to fostering cutting-edge knowledge and practical skills in this transformative field. Our programs delve into the molecular basis of cancer therapeutics, providing comprehensive insights into advanced drug delivery systems, gene therapy, and the latest innovations in biotechnology and molecular biology relevant to oncology. By participating in our specialized courses, you gain access to expert-led training, hands-on experience, and a deep understanding of how to translate groundbreaking scientific discoveries into tangible solutions for patients. Join us to be at the forefront of the fight against cancer, contributing to a future where targeted, effective, and less toxic treatments are the norm.
Join Now
Frequently Asked Questions (FAQ)
What is targeted drug delivery in cancer treatment?
Targeted drug delivery in cancer treatment involves using specific carriers, often nanoparticles, to deliver therapeutic agents directly to cancer cells or tumor sites, minimizing exposure to healthy tissues. This approach aims to increase drug efficacy and reduce systemic side effects associated with conventional therapies like chemotherapy.
How does nanotechnology help in cancer diagnostics?
Nanotechnology significantly enhances cancer diagnostics by enabling the development of highly sensitive biosensors for early detection of biomarkers, and advanced imaging agents (like quantum dots or gold nanoparticles) that provide clearer, more precise visualization of tumors and metastases. This allows for earlier intervention and more accurate monitoring of disease progression.
What are the main types of nanocarriers used for cancer drug delivery?
Common types of nanocarriers used for cancer drug delivery include liposomes, polymeric nanoparticles, dendrimers, and various inorganic nanoparticles (e.g., gold, magnetic). Each type has unique properties that can be exploited for specific drug encapsulation, release profiles, and targeting strategies, contributing to diverse approaches in cancer research.
How do Deep Science Workshops contribute to advancements in oncology?
Deep Science Workshops and Deep Science Implementation play a crucial role by offering specialized training and educational programs focused on cutting-edge fields like nanotechnology, molecular biology, gene therapy, and advanced biotechnology relevant to oncology. They equip students and professionals with the knowledge and practical skills needed to contribute to innovative cancer research and the development of next-generation cancer therapeutics.