The Foundation of Trust: Patient Consent and Autonomy in Clinical Trials
At the heart of any ethical discussion in cancer research lies the principle of informed consent. Patients participating in clinical trials, which are crucial for advancing cancer therapy, must fully understand the purpose, procedures, potential risks, and benefits of the research. This is particularly vital in oncology, where patients are often vulnerable and facing life-threatening conditions. Ensuring genuine autonomy means providing comprehensive information in an understandable format, allowing patients to make voluntary decisions free from coercion. This includes the right to withdraw at any time without penalty. The ethical conduct of clinical trials is a cornerstone for the credibility of new drug discovery and the validation of novel treatments like immunotherapy, ensuring that human dignity is upheld throughout the rigorous process of testing and validation.
Safeguarding Sensitive Information: Data Privacy and Confidentiality
The explosion of 'omics' data – genomics, proteomics, metabolomics – has revolutionized cancer genetics and molecular biology. Researchers now have access to unprecedented amounts of patient data, which can lead to breakthroughs in identifying new biomarkers and understanding disease progression. However, this wealth of information comes with significant ethical challenges regarding data privacy and confidentiality. Protecting patient identities and sensitive health information is paramount to prevent misuse, discrimination, or unauthorized access. Robust data governance frameworks, anonymization techniques, and secure data storage are not just technical requirements but ethical imperatives. The responsible handling of data builds trust, encouraging more individuals to contribute to vital oncology research and accelerating the pace of personalized cancer therapy.
Equitable Access and Benefit Sharing: A Global Responsibility
As new cancer therapy breakthroughs emerge, a critical ethical question arises: who benefits from these advancements? The disparity in access to cutting-edge treatments and participation in cancer research between high-income and low-income countries, or even within different socioeconomic groups in the same country, is a significant ethical concern. Ensuring equitable access to new drugs, diagnostic tools, and clinical trials is a global responsibility. Furthermore, ethical considerations extend to benefit sharing, especially when research involves populations from developing countries or utilizes traditional knowledge. The goal of oncology research should be to alleviate suffering universally, not just for a privileged few. This principle also extends to the accessibility of biotechnology jobs, ensuring a diverse and inclusive workforce that can address global health challenges.
Integrity and Transparency: The Bedrock of Scientific Progress
Maintaining scientific integrity and transparency is fundamental to all cancer research. This includes accurate reporting of results, whether positive or negative, avoiding selective publication, and ensuring proper attribution of intellectual contributions. Research misconduct, such as falsification or fabrication of data, not only undermines public trust but also jeopardizes patient safety and misdirects future research efforts in drug discovery and gene therapy. Ethical guidelines demand rigorous peer review, clear conflict of interest policies, and open access to research findings where appropriate. For professionals in biotechnology jobs, upholding these standards is not just a professional duty but a moral obligation to advance science responsibly.
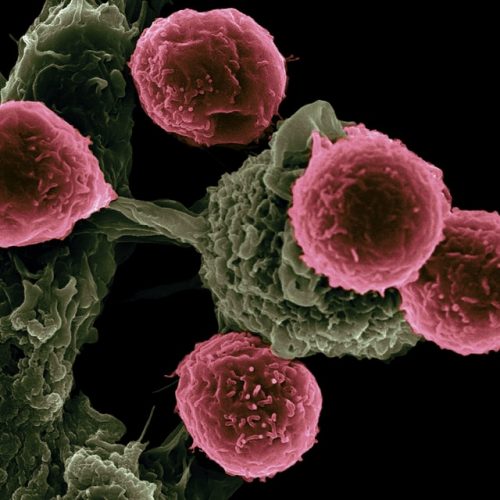
The Ethical Frontier: Emerging Technologies in Cancer Research
The rapid evolution of technologies like CRISPR-Cas9 for gene therapy, advanced AI in drug discovery, and sophisticated imaging for biomarker identification presents new ethical dilemmas. While these innovations hold immense promise for cancer therapy, their application requires careful ethical scrutiny. For instance, germline gene editing raises profound questions about altering the human genome for future generations. The use of AI in diagnostics and treatment planning necessitates discussions around bias in algorithms and accountability. Similarly, the development of complex immunotherapy approaches, while revolutionary, requires continuous monitoring for unforeseen long-term effects. Engaging in proactive ethical discourse and establishing clear regulatory frameworks are essential to harness the power of these technologies responsibly for oncology research.
Animal Welfare in Pre-clinical Research
Before any new cancer therapy or drug discovery enters human clinical trials, extensive pre-clinical research often involves animal models. Ethical considerations surrounding animal welfare are crucial in this phase of cancer research. The "3Rs" principle – Replacement (using non-animal methods where possible), Reduction (minimizing the number of animals used), and Refinement (improving animal welfare and minimizing suffering) – guides responsible animal experimentation. Adhering to these principles ensures that essential scientific insights are gained while treating research animals with the utmost care and respect. This careful balance is vital for the foundational work in molecular biology and cancer genetics that underpins future human treatments.
Commercialization and Conflicts of Interest
The journey from a scientific breakthrough in oncology research to a marketable cancer therapy often involves significant financial investment and commercial interests. This can lead to potential conflicts of interest for researchers, institutions, and pharmaceutical companies. Ethical guidelines require transparency regarding funding sources, financial ties, and intellectual property. The primary motivation for cancer research should always be the well-being of patients and the advancement of public health, not solely profit. Striking an ethical balance between innovation, accessibility, and commercial viability is a complex but necessary challenge in the biotechnology sector, impacting everything from drug discovery pipelines to the availability of new biomarkers.
Shaping the Future: Education and Ethical Training in Biotechnology
To navigate these complex ethical landscapes, continuous education and training are indispensable for anyone involved in cancer research, from aspiring scientists to seasoned professionals in biotechnology jobs. Programs like the "Molecular Basis of Cancer Therapeutics and Targets" offered by Deep Science Workshops and Deep Science Implementation are crucial. These initiatives not only impart cutting-edge knowledge in molecular biology, cancer genetics, gene therapy, and immunotherapy but also embed a strong ethical foundation. Understanding the scientific intricacies of cancer therapy goes hand-in-hand with understanding the moral responsibilities that accompany such powerful knowledge. By fostering a culture of ethical awareness, we ensure that the next generation of researchers is equipped to make responsible decisions that benefit all of humanity.
The relentless pursuit of cures for cancer is a testament to human ingenuity and perseverance. However, this pursuit must always be guided by a steadfast commitment to ethical principles. By prioritizing patient well-being, ensuring data privacy, promoting equitable access, upholding research integrity, and thoughtfully navigating emerging technologies, the field of cancer research can continue to deliver transformative cancer therapy solutions responsibly. The ethical landscape is dynamic, requiring ongoing dialogue, adaptation, and a collective dedication from all stakeholders – researchers, clinicians, policymakers, and the public – to ensure that scientific progress truly serves the greater good.
Join Now