In the relentless global fight against cancer, clinical trials stand as the bedrock of progress. They are the critical bridge translating groundbreaking scientific discoveries from the laboratory into life-saving treatments for patients. For anyone involved in cancer research, oncology, or the broader biotechnology and biopharma industries, a deep understanding of clinical trial design in oncology is not merely beneficial—it is absolutely essential. This comprehensive guide will help you understand the principles of clinical trial design in oncology, exploring the intricate methodologies, ethical considerations, and strategic approaches that underpin successful studies in this complex field. From the initial conceptualization to the final analysis, every stage of a clinical trial demands precision, foresight, and adherence to rigorous standards to ensure valid and impactful results in the quest for improved cancer therapy.
At its heart, robust clinical trial design is about minimizing bias and maximizing the ability to detect a true treatment effect. Several core principles guide this process, ensuring the integrity and validity of studies in oncology.
Every clinical trial begins with clear, measurable objectives. These define what the trial aims to achieve. Primary objectives typically focus on the main question, such as whether a new drug improves overall survival or progression-free survival in a specific cancer type. Secondary objectives explore additional benefits or safety profiles. Corresponding endpoints are the specific measurements used to assess these objectives. For instance, in oncology, common endpoints include overall survival (OS), progression-free survival (PFS), objective response rate (ORR), and duration of response (DOR). Carefully chosen endpoints are crucial for generating meaningful data for evaluating new cancer therapy options.
Selecting the right patient population is paramount. Eligibility criteria define who can and cannot participate in the trial, ensuring homogeneity within the study group and minimizing confounding factors. These criteria are meticulously crafted based on the disease stage, previous treatments, comorbidities, and performance status. This careful selection ensures that the results are generalizable to the target patient population while prioritizing patient safety within the context of cancer research.
To ensure unbiased comparison between treatment arms, randomization is a cornerstone of good design. Patients are randomly assigned to receive either the experimental treatment or a control (e.g., placebo, standard of care). Blinding (or masking) further reduces bias by preventing patients, investigators, or both from knowing which treatment arm a patient is in. Single-blinding (patient unaware) or double-blinding (both patient and investigator unaware) are common, though sometimes challenging in complex cancer regimens.
A control arm provides a baseline for comparison, allowing researchers to determine if the experimental treatment offers a significant advantage. The choice of control (e.g., placebo, active comparator, standard of care) depends on the ethical considerations and the existing treatment landscape. Furthermore, sample size calculation is critical to ensure adequate statistical power—the probability of detecting a true effect if one exists. Underpowered studies can lead to false negative results, hindering the development of promising cancer treatments.
Clinical trials in oncology typically progress through a series of phases, each with distinct objectives, meticulously designed to assess safety and efficacy:
The field of cancer research is dynamic, and so are its trial designs. Modern clinical studies often incorporate advanced methodologies to accelerate findings and improve patient outcomes:
Adaptive designs allow for pre-specified modifications to the trial design based on accumulating data, making trials more efficient and ethical. This could involve adjusting sample sizes, dropping ineffective arms, or changing randomization ratios, accelerating the path to effective treatments.
With advances in molecular biology and genomics, many oncology trials are now biomarker-driven. Patients are selected based on the presence of specific genetic mutations or protein expressions that predict response to targeted therapies. This precision approach is revolutionizing cancer treatment by matching the right therapy to the right patient.
These innovative designs are particularly relevant in precision oncology. Basket trials test one drug across multiple cancer types, all sharing a common genetic alteration. Umbrella trials test multiple drugs for a single cancer type, stratifying patients by specific biomarkers. These designs streamline drug discovery and development processes.
All clinical trials are governed by strict ethical and regulatory guidelines to protect patient rights and ensure data integrity. Key components include:
The synergy between biotechnology and oncology is undeniable. Breakthroughs in biological sciences have paved the way for entirely new classes of cancer therapy, transforming treatment paradigms:
A deep understanding of cancer at the molecular biology level has enabled the identification of specific genetic mutations, signaling pathways, and protein targets unique to cancer cells. This knowledge is the foundation for developing highly targeted therapies, moving away from broad-spectrum chemotherapy towards more precise interventions. This forms the very basis of modern drug discovery in oncology.
The advent of gene therapy offers revolutionary approaches, from correcting genetic defects that cause cancer to engineering immune cells to fight tumors. These complex therapies require specialized clinical trial design to assess their safety and efficacy, often involving intricate delivery systems and long-term follow-up.
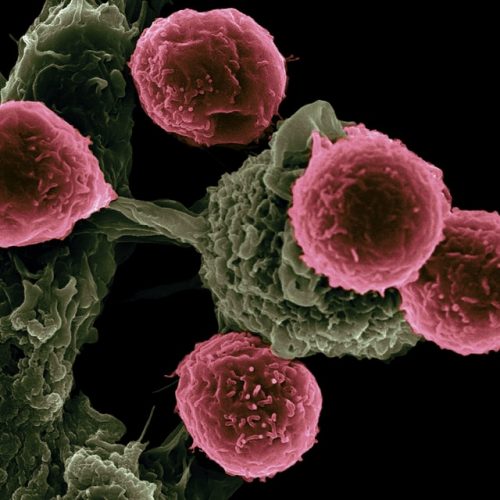
Perhaps one of the most transformative advancements in recent cancer research is immunotherapy. By harnessing the body's own immune system to recognize and destroy cancer cells, immunotherapies have delivered unprecedented responses in various cancers. Designing trials for immunotherapies involves unique considerations, such as pseudoprogression and delayed responses, which differ from traditional cytotoxic agents.
The entire pipeline of drug discovery, from preclinical screening to late-stage development, is driven by innovations in biotechnology. The biopharma industry invests heavily in research and development, translating scientific insights into investigational new drugs. Their expertise in manufacturing, regulatory affairs, and large-scale clinical studies is indispensable for bringing new cancer treatment options to patients worldwide.
Effective data management is critical for the success of any clinical trial. This involves meticulous collection, cleaning, and storage of vast amounts of patient data. Robust statistical analysis is then applied to interpret these data, drawing meaningful conclusions about a treatment's efficacy and safety. The insights gained from these analyses form the basis for regulatory submissions to agencies like the FDA or EMA. These submissions are comprehensive dossiers detailing every aspect of the trial, from design and conduct to results and safety profiles. A well-prepared submission is crucial for securing approval and making new therapies available to patients.
Despite significant advancements, clinical trials in oncology face ongoing challenges, including patient recruitment, high costs, and the complexity of data management. However, the future is bright with emerging trends:
These innovations promise to make future clinical studies even more efficient, patient-centric, and impactful in the ongoing battle against cancer.
To truly understand the principles of clinical trial design in oncology is to grasp the engine driving progress in cancer research. From foundational statistical concepts to cutting-edge applications of biotechnology, each element plays a vital role in bringing effective cancer therapy to those who need it most. Professionals in oncology, biopharma, and related fields must continually update their knowledge to navigate this evolving landscape. Equipping oneself with comprehensive expertise in clinical trial design is not just about professional development; it's about contributing directly to a future where cancer is a manageable, if not curable, disease. For those looking to deepen their expertise and contribute meaningfully to this critical domain, specialized programs like those offered by Deep Science Workshops and Deep Science Implementation provide invaluable pathways to mastering these complex principles.
Join Now: Advance Your Expertise in Molecular Basis of Cancer Therapeutics and TargetsThe primary objectives of clinical trials in oncology are to evaluate the safety, efficacy, and optimal dosage of new treatments, and to compare them against existing therapies or placebos. They aim to determine if a new intervention can improve patient outcomes, such as survival, quality of life, or disease progression.
Biotechnology plays a pivotal role in advancing cancer therapy by enabling the discovery of novel therapeutic targets, developing precision medicines, engineering immunotherapies like CAR T-cells, and facilitating gene therapy approaches. It underpins the entire drug discovery pipeline, from preclinical research to clinical development.
Understand the principles of clinical trial design in oncology is crucial for professionals in cancer research because it ensures the generation of reliable, statistically sound, and ethically conducted studies. Proper design minimizes bias, maximizes the chances of detecting true treatment effects, and ultimately accelerates the translation of scientific discoveries into effective cancer therapies for patients.
Both are innovative clinical trial design types. A basket trial tests one drug across multiple cancer types, all sharing a specific genetic mutation or biomarker. An umbrella trial, conversely, tests multiple drugs for a single cancer type, stratifying patients into subgroups based on their specific biomarkers to receive different targeted therapies.
Molecular biology is fundamental to modern cancer drug discovery. It allows researchers to delve into the genetic and molecular underpinnings of cancer, identifying specific oncogenes, tumor suppressor genes, and signaling pathways that drive cancer growth. This detailed understanding enables the design of highly targeted drugs and precision medicine approaches, significantly impacting the development of new cancer therapy.