The Imperative of Regulation in Cancer Research
The complexity of cancer, coupled with the potent nature of its treatments, necessitates a robust regulatory framework. Every new cancer therapy, whether it's a small molecule drug, a biologic, or a cellular therapy, must undergo rigorous testing to prove its safety and effectiveness. Without these regulations, the market could be flooded with unproven or even harmful substances, jeopardizing patient lives and eroding confidence in medical science. Regulatory bodies worldwide, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), serve as gatekeepers, ensuring that only thoroughly vetted treatments reach the public.
These regulations cover every phase of drug development, from preclinical studies in laboratories and animal models to multi-phase clinical trials involving human subjects. Adherence to Good Laboratory Practice (GLP), Good Clinical Practice (GCP), and Good Manufacturing Practice (GMP) is not optional; it's the bedrock upon which successful drug development is built. For institutions engaged in advanced scientific training, like those offering Deep Science Workshops, emphasizing these regulatory aspects is crucial for future researchers and developers.
Key Regulatory Bodies and Their Roles
Several national and international bodies oversee the development and approval of cancer drugs. The FDA is perhaps the most well-known in the United States, with its Center for Drug Evaluation and Research (CDER) and Center for Biologics Evaluation and Research (CBER) playing critical roles. In Europe, the EMA performs a similar function, harmonizing regulatory standards across member states. Other significant bodies include the Pharmaceuticals and Medical Devices Agency (PMDA) in Japan and the National Medical Products Administration (NMPA) in China.
Each agency has specific guidelines for different types of therapies. For instance, the regulatory pathway for a conventional chemotherapy drug differs significantly from that of a novel gene therapy or a complex immunotherapy. These agencies provide guidance documents, conduct inspections, and ultimately grant or deny marketing approval based on comprehensive data submissions. Navigating these diverse requirements is a core challenge for any pharmaceutical or biotech company.
Stages of Drug Development and Regulatory Milestones
The journey of a new cancer therapy from concept to clinic is long and arduous, marked by several regulatory milestones:
- Discovery and Preclinical Research: This initial phase involves identifying potential drug candidates and conducting laboratory and animal studies to assess their biological activity, toxicity, and pharmacokinetic properties. Regulatory oversight here ensures ethical animal use and data integrity.
- Investigational New Drug (IND) Application: Before human trials can begin, researchers must submit an IND application to the relevant regulatory authority. This comprehensive document details preclinical data, manufacturing information, and the proposed clinical trial protocol. Approval of an IND allows the drug to be tested in humans.
- Clinical Trials (Phases I, II, III):
- Phase I: Small group of healthy volunteers or patients to assess safety, dosage, and side effects.
- Phase II: Larger group of patients to evaluate efficacy and further assess safety.
- Phase III: Large-scale trials comparing the new treatment to existing therapies or placebo, confirming efficacy and monitoring adverse effects.
- New Drug Application (NDA) / Biologics License Application (BLA): Upon successful completion of clinical trials, the company submits an NDA (for small molecules) or BLA (for biologics like immunotherapy or gene therapy) to seek marketing approval. This application includes all data collected throughout development.
- Post-Market Surveillance: Even after approval, drugs are continuously monitored for long-term safety and efficacy through pharmacovigilance programs. Regulatory bodies may require post-market studies or even withdraw a drug if new safety concerns arise.
Specific Regulatory Considerations for Gene Therapy and Immunotherapy
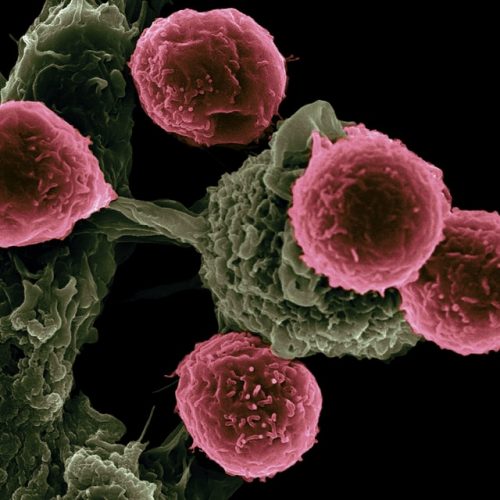
The advent of gene therapy and immunotherapy has revolutionized oncology, offering unprecedented hope for patients. However, these advanced biotechnology approaches also present unique regulatory challenges due to their complex mechanisms of action and potential for long-term effects. Regulators must grapple with questions of viral vector safety, gene editing off-target effects, and the potential for immune-related adverse events. Specialized guidelines have been developed to address these concerns, reflecting the cutting-edge nature of these treatments and the need for meticulous oversight.
For instance, CAR T-cell therapies, a form of immunotherapy, involve genetically modifying a patient's own cells. This requires strict controls over cell collection, manufacturing, and administration, often under the purview of both drug and tissue/cell product regulations. The precision required in molecular biology techniques used in these therapies demands equally precise regulatory frameworks.
Challenges in Regulatory Compliance for Biotechnology and Pharmaceutical Companies
Compliance with global regulations is a significant undertaking for any pharmaceutical or biotech firm. The challenges include:
- Evolving Landscape: Regulations are constantly updated to keep pace with scientific advancements, especially in rapidly moving fields like cancer research.
- Global Harmonization: Differences in regulatory requirements across countries can complicate multinational clinical trials and drug approvals.
- Data Management: The sheer volume of data generated during drug development requires robust systems for collection, analysis, and submission.
- Cost and Time: Regulatory compliance adds substantial cost and time to the drug development process, which can be particularly burdensome for smaller biotech startups.
- Ethical Considerations: Ensuring ethical conduct in human trials, especially for vulnerable patient populations, is a continuous challenge.
To overcome these, companies often invest heavily in regulatory affairs departments and seek expert guidance. Programs like Deep Science Implementation are vital for training the next generation of professionals to navigate these complexities effectively.
The Role of Molecular Biology in Modern Cancer Drugs Development
At the heart of modern cancer therapy development is molecular biology. Understanding the genetic and molecular underpinnings of cancer allows for the design of highly targeted therapies that interfere with specific pathways driving tumor growth. This precision medicine approach has led to the development of drugs that are more effective and have fewer side effects than traditional chemotherapy.
Regulatory bodies are increasingly focusing on the molecular characteristics of tumors, often requiring companion diagnostics to identify patients most likely to benefit from a particular targeted cancer drug. This integration of diagnostics and therapeutics, known as theranostics, adds another layer of regulatory complexity but promises more personalized and effective oncology treatments.
Ensuring Ethical Practices in Oncology
Beyond efficacy and safety, ethical considerations are paramount in cancer research. Regulations ensure that patient rights are protected, informed consent is obtained, and vulnerable populations are not exploited. Institutional Review Boards (IRBs) or Ethics Committees play a crucial role in reviewing and approving clinical trial protocols, ensuring they meet ethical standards. This commitment to ethical practice is a cornerstone of responsible cancer therapy development.
The Future of Cancer Therapy Regulations
The future of regulations in cancer research will likely see continued adaptation to rapid scientific progress. There will be an increasing emphasis on real-world evidence, adaptive trial designs, and expedited pathways for breakthrough therapies. International collaboration among regulatory agencies is also expected to grow, aiming for greater harmonization and efficiency in bringing innovative cancer drugs to patients globally. The goal remains constant: to accelerate the availability of safe and effective treatments while maintaining the highest standards of oversight.
Conclusion
Understanding the regulations involved in cancer research is not just a matter of compliance; it's about safeguarding public health and accelerating the delivery of life-saving innovations. From the foundational principles of biotechnology and molecular biology to the complex clinical trials of gene therapy and immunotherapy, every step in developing a new cancer therapy is meticulously governed. For aspiring professionals in oncology and the pharmaceutical industry, mastering this regulatory landscape is as crucial as scientific discovery itself.
As the field of cancer research continues to evolve, so too will the regulatory frameworks. Staying informed and engaged with these developments is essential for anyone committed to advancing the fight against cancer. For those looking to deepen their understanding and practical skills in this vital area, consider exploring specialized programs and workshops that bridge the gap between cutting-edge science and regulatory expertise.
Join NowFrequently Asked Questions About Cancer Research Regulations
Why are regulations crucial in cancer research?
Regulations are crucial in cancer research to ensure patient safety, efficacy of new treatments, ethical conduct of studies, and to maintain public trust. They standardize processes from preclinical testing to clinical trials and post-market surveillance, ensuring that only safe and effective cancer drugs reach patients.
What role does biotechnology play in developing new cancer therapies?
Biotechnology is at the forefront of developing innovative cancer therapy approaches, including targeted therapies, gene therapy, and immunotherapy. It leverages biological systems and organisms to create new diagnostic tools and treatments, pushing the boundaries of what's possible in oncology.
How do regulatory bodies impact the approval process for cancer treatments?
Regulatory bodies like the FDA in the US or EMA in Europe meticulously review data from preclinical and clinical trials. They assess the safety, efficacy, and quality of new cancer drugs. Their stringent approval process ensures that only well-vetted treatments are made available to the public, significantly impacting the timeline and success of bringing a new cancer therapy to market.