The Paradigm Shift: Understanding Immunotherapy in Cancer Therapy
At its core, immunotherapy represents a fundamental re-evaluation of how we approach cancer therapy. Instead of directly attacking cancerous cells, which often leads to collateral damage to healthy tissues, immunotherapies work by either stimulating the patient's existing immune response or by introducing engineered immune components. This strategic shift leverages the immune system's inherent ability to distinguish between healthy and diseased cells, offering a more targeted and potentially less toxic treatment option. The development of these therapies has been a testament to profound insights gained through intensive cancer research and breakthroughs in molecular biology, revealing the complex interplay between tumors and the immune microenvironment. Understanding these mechanisms is paramount for anyone involved in oncology or drug discovery.
Key Modalities of Advanced Immunotherapies
The landscape of immunotherapy is diverse and rapidly expanding, with several key modalities showing remarkable promise in cancer treatment:
Checkpoint Inhibitors: Unleashing the Immune System
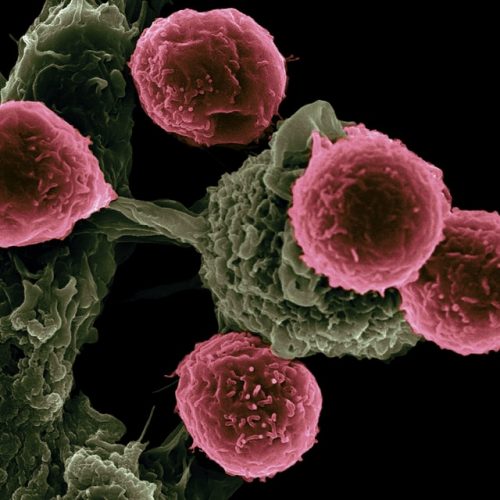
Perhaps the most widely recognized form of immunotherapy, checkpoint inhibitors work by blocking proteins (like PD-1, PD-L1, and CTLA-4) that cancer cells use to 'hide' from the immune system. By disabling these "checkpoints," these drugs effectively remove the brakes from the immune response, allowing T-cells to recognize and attack tumor cells. This breakthrough has revolutionized the treatment of various cancers, including melanoma, lung cancer, and kidney cancer, demonstrating the profound impact of targeted drug discovery.
CAR T-cell Therapy: Engineering Precision Killers
Chimeric Antigen Receptor (CAR) T-cell therapy is a sophisticated form of gene therapy where a patient’s own T-cells are genetically engineered in the lab to express a CAR that specifically targets antigens on cancer cells. These modified T-cells are then infused back into the patient, where they act as living drugs, seeking out and destroying cancer. This highly personalized approach has shown remarkable success in certain blood cancers, showcasing the immense potential of integrating molecular biology with clinical application.
Oncolytic Viruses and Cancer Vaccines: Emerging Frontiers
Oncolytic viruses are naturally occurring or genetically modified viruses that preferentially infect and kill cancer cells, while also stimulating an anti-tumor immune response. Cancer vaccines, on the other hand, aim to prime the immune system to recognize and attack cancer cells, either preventatively or therapeutically. These modalities, along with others, are continuously being explored through rigorous clinical trials, expanding the arsenal of cancer therapy options.
The Crucial Role of Molecular Biology and Biomarkers
The success of modern immunotherapy is deeply intertwined with our understanding of molecular biology. Cancer is not a single disease but a collection of diseases driven by specific genetic and molecular alterations. Identifying these unique molecular signatures is vital for predicting which patients will respond to certain immunotherapies and for developing new, more effective treatments. This is where biomarkers come into play. Biomarkers are measurable indicators of a biological state or condition, used to diagnose disease, assess prognosis, and predict response to therapy. For example, PD-L1 expression is a key biomarker used to guide treatment decisions for checkpoint inhibitors. The ongoing quest for novel biomarkers is a significant area of cancer research, enabling personalized oncology and optimizing treatment strategies.
From Discovery to Clinic: The Journey of Drug Discovery and Clinical Trials
The journey of a new immunotherapy from a laboratory concept to a life-saving treatment is long and complex, involving extensive drug discovery and rigorous clinical trials. It begins with fundamental cancer research, where scientists identify potential targets and mechanisms. Promising candidates then move through preclinical testing, followed by multiple phases of clinical trials in human patients. These trials are essential for evaluating the safety, efficacy, and optimal dosing of new therapies. The data gathered from these trials, meticulously analyzed by experts in biotechnology and oncology, dictates whether a new treatment can be approved for widespread use. This iterative process of research, development, and validation underscores the collaborative efforts required to advance cancer therapy.
The Future Landscape: Gene Therapy and Beyond
The field of immunotherapy is still in its nascent stages, with incredible potential yet to be fully realized. Future directions include the development of novel combination therapies, integrating immunotherapy with traditional treatments or other targeted therapies. Advances in gene therapy are paving the way for even more sophisticated engineered cell therapies. Furthermore, ongoing cancer research is focused on understanding mechanisms of resistance to immunotherapy, identifying new targets, and developing strategies to make these treatments effective for a broader range of cancers and patients. The continuous evolution of biotechnology promises a future where cancer is increasingly manageable, and for many, a curable disease.
Empowering the Next Generation: The Need for Specialized Education
The rapid pace of innovation in immunotherapy and cancer research demands a highly skilled and knowledgeable workforce. Professionals in biotechnology, oncology, molecular biology, and drug discovery must stay abreast of the latest developments, from understanding complex immune pathways to interpreting the results of clinical trials. Specialized education is not just beneficial; it is imperative for those aiming to contribute meaningfully to this dynamic field. An advanced cancer immunotherapy course provides the foundational knowledge and practical insights necessary to navigate the complexities of modern cancer therapy, fostering a deeper understanding of the molecular basis of these revolutionary treatments.
Deep Science Workshops: Your Gateway to Expertise
Recognizing this critical need for specialized knowledge, Deep Science Workshops offers comprehensive programs designed to equip aspiring and current professionals with the expertise required in the evolving landscape of cancer therapeutics. Our courses delve into the intricacies of molecular biology, the latest advancements in immunotherapy, and the practical aspects of drug discovery and clinical trials. Through immersive learning experiences and hands-on insights, participants gain a profound understanding of how basic cancer research translates into life-saving treatments. With a focus on practical application and cutting-edge information, Deep Science Implementation ensures that our learners are at the forefront of innovation, ready to make significant contributions to the future of oncology.
Join Our Advanced Cancer Immunotherapy Course Now
Frequently Asked Questions (FAQs) about Cancer Immunotherapy
What is cancer immunotherapy?
Cancer immunotherapy is a revolutionary approach to cancer therapy that harnesses the power of the body's own immune system to identify and destroy cancer cells. Unlike traditional treatments like chemotherapy or radiation, which directly attack cancer cells, immunotherapy works by boosting the immune system's natural defenses or by introducing engineered immune components to target cancer specifically. This includes modalities like checkpoint inhibitors, CAR T-cell therapy, and cancer vaccines, representing significant advancements in oncology.
Why is understanding molecular biology crucial for cancer therapeutics?
Understanding molecular biology is absolutely crucial for modern cancer therapeutics because cancer itself is a disease driven by molecular abnormalities. Deep knowledge of cellular pathways, genetic mutations, and protein interactions allows researchers to identify specific targets for new drugs, develop precise biomarkers for diagnosis and treatment response, and engineer advanced therapies like gene therapy and CAR T-cells. This foundational knowledge is essential for effective drug discovery and guiding personalized medicine in cancer research and clinical trials.