What are Cancer Biomarkers and Why Are They Crucial?
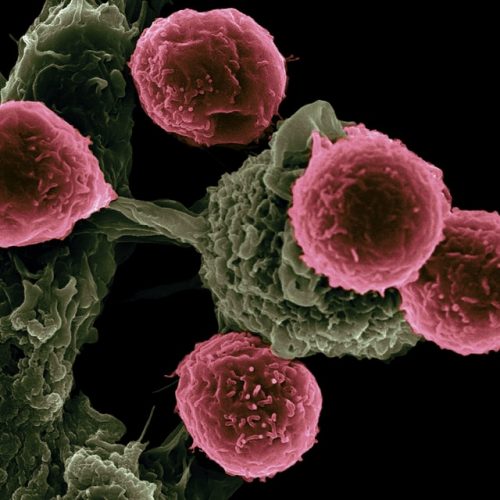
Cancer biomarkers are measurable indicators of a biological state. In the context of oncology, they can be molecules, cells, or genes that are produced by the tumor itself or by other cells in response to cancer. Their significance spans across various aspects of cancer management:
- Early Detection: Identifying cancer at its nascent stages, often before symptoms appear, dramatically improves prognosis.
- Diagnosis and Prognosis: Helping to confirm a diagnosis, classify tumor types, and predict disease aggressiveness or patient outcome.
- Predictive Biomarkers: Forecasting a patient's likely response to a specific cancer therapy, enabling personalized treatment plans.
- Monitoring Treatment Response: Tracking the effectiveness of therapies and detecting recurrence early.
- Drug Development: Accelerating drug discovery by identifying molecular targets and stratifying patients for clinical trials.
The utility of a marker is directly proportional to its specificity and sensitivity, making the identification and validation process critical for their clinical adoption. This is where cutting-edge biotechnology and meticulous molecular biology techniques come into play.
The Rigorous Process of Biomarker Identification
The journey to identify novel cancer biomarkers typically begins in the discovery phase, often leveraging high-throughput 'omics' technologies. This phase aims to cast a wide net, searching for molecular differences between cancerous and healthy tissues or bodily fluids to identify potential indicators.
1. Discovery Phase: Leveraging 'Omics' Technologies
Modern cancer research relies heavily on advanced techniques to uncover potential biomarkers:
- Genomics and Transcriptomics: Analyzing DNA mutations, gene amplifications, deletions, and altered gene expression (RNA levels). Techniques like Next-Generation Sequencing (NGS) and microarray analysis are fundamental here. For instance, specific gene mutations can serve as predictive biomarkers for targeted cancer therapy.
- Proteomics: Studying the entire set of proteins expressed by cells or tissues. Mass spectrometry-based proteomics can identify differentially expressed proteins, post-translational modifications, and protein-protein interactions that are unique to cancer. These protein markers are often more directly linked to cellular function and disease phenotype.
- Metabolomics: Examining small molecule metabolites in biological samples. Changes in metabolic pathways are a hallmark of cancer, and specific metabolic profiles can serve as diagnostic or prognostic indicators.
- Epigenomics: Investigating epigenetic modifications like DNA methylation and histone modifications, which play a crucial role in gene regulation and can be altered in cancer.
Beyond these, emerging fields like liquid biopsies, which analyze circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and exosomes from blood, are revolutionizing non-invasive biomarker discovery in cancer research. This approach holds immense promise for early detection and real-time monitoring of disease progression and treatment response.
Validating the Promise: From Candidate to Clinic
Identifying a potential biomarker is only the first step. For a biomarker to be clinically useful, it must undergo rigorous validation to ensure its reliability, accuracy, and clinical utility. This multi-stage process is critical for translating discoveries from the lab to patient care.
1. Analytical Validation
This stage assesses the technical performance of the biomarker assay. It ensures that the measurement method is robust, reproducible, and accurate. Key parameters include:
- Sensitivity: The lowest amount of the biomarker that can be reliably detected.
- Specificity: The ability to accurately measure the target biomarker without interference from other substances.
- Reproducibility: Consistent results when the test is performed multiple times, by different operators, or in different laboratories.
- Accuracy: How close the measured value is to the true value.
High-quality analytical validation is paramount, as errors at this stage can lead to misleading clinical results. This phase often involves extensive work in advanced biotechnology labs.
2. Clinical Validation
Once an assay is analytically validated, its clinical utility must be established. This involves demonstrating that the biomarker provides meaningful information for patient management. Clinical validation typically proceeds in stages:
- Retrospective Studies: Using archived patient samples with known clinical outcomes to assess the biomarker's ability to distinguish between disease states or predict outcomes.
- Prospective Studies: The gold standard, involving collecting samples from patients over time and correlating biomarker levels with disease progression, treatment response, or survival. These studies are essential for confirming the biomarker's predictive or prognostic value in a real-world setting.
- Clinical Utility: Demonstrating that using the biomarker leads to improved patient outcomes or more cost-effective healthcare. This is the ultimate goal of biomarker discovery in cancer research.
The statistical rigor applied during clinical validation is immense, involving large cohorts and sophisticated analytical methods to ensure the observed associations are statistically significant and clinically relevant. This iterative process often involves collaboration between clinical oncology teams and molecular biology experts.
Challenges and Future Directions in Biomarker Research
Despite significant progress, the field of cancer biomarkers faces several challenges. These include the inherent heterogeneity of tumors, the low abundance of some biomarkers in early-stage disease, and the complexity of validating multi-biomarker panels. Furthermore, regulatory hurdles and the need for standardized assays add to the complexity.
However, the future of biomarker discovery in cancer research is incredibly promising. Advances in artificial intelligence and machine learning are enabling the analysis of vast datasets to identify complex biomarker signatures. The rise of liquid biopsies offers non-invasive, repeatable sampling, making it easier to monitor disease and treatment response over time, and identify new markers. Integration of multi-omics data (genomics, proteomics, metabolomics) promises a more comprehensive understanding of cancer biology and the identification of highly specific and sensitive indicators.
These advancements are not just theoretical; they are directly impacting cancer therapy. For instance, the identification of specific genetic mutations has led to the development of targeted drugs, a prime example of personalized cancer therapy. Similarly, understanding immune checkpoint biomarkers has revolutionized immunotherapy, offering new hope for patients with previously untreatable cancers. The continuous cycle of biomarker identification, validation, and clinical application is central to modern drug discovery and the evolution of precision oncology.
Deep Science Workshops and Deep Science Implementation are at the forefront of educating the next generation of scientists and researchers in these critical areas, ensuring that the knowledge and skills required to advance biomarker research are widely accessible.
Join Now: Advance Your Expertise in Molecular Basis of Cancer Therapeutics and TargetsFrequently Asked Questions about Cancer Biomarkers
What is the primary goal of cancer biomarker identification?
The primary goal of cancer biomarker identification is to find specific molecular indicators that can be used for early detection, accurate diagnosis, prognosis prediction, and to guide personalized cancer therapy. These biomarkers are crucial for improving patient outcomes and streamlining drug discovery in oncology.
How does biotechnology contribute to biomarker discovery?
Biotechnology provides the advanced tools and techniques necessary for biomarker discovery in cancer research. This includes high-throughput sequencing (genomics), mass spectrometry (proteomics), and sophisticated analytical platforms that enable the comprehensive analysis of biological samples to identify potential biomarkers. It's fundamental to advancements in molecular biology applied to cancer.
What is the difference between analytical and clinical validation of a biomarker?
Analytical validation assesses the technical performance of the biomarker assay itself, ensuring it is accurate, precise, and reproducible. Clinical validation, on the other hand, evaluates the biomarker's ability to provide meaningful clinical information, such as predicting disease progression, treatment response, or patient survival, in actual patient populations. Both are essential steps before a biomarker can be used in clinical practice for cancer therapy.
Can biomarkers help with personalized cancer therapy?
Absolutely. Biomarkers are central to personalized cancer therapy. By identifying specific genetic mutations or protein expressions in a patient's tumor, clinicians can select targeted drugs or immunotherapy treatments that are most likely to be effective, minimizing side effects and maximizing therapeutic benefit. This approach optimizes treatment strategies in oncology.