In the relentless battle against cancer, clinical trials stand as the vanguard of progress, transforming scientific breakthroughs into tangible hope for millions. These meticulously designed studies are the bridge between laboratory discoveries and life-saving treatments, representing a critical phase in the journey of every new therapy. From groundbreaking insights in molecular biology to the cutting-edge applications of biotechnology, the landscape of cancer treatment is constantly evolving, driven by the dedication of researchers and the courage of patients.
This article delves deep into the multifaceted world of clinical trials in cancer research, exploring their rigorous process, the innovative therapies they evaluate, and the profound impact they have on shaping the future of cancer therapy. We will uncover how drug discovery and development intertwine with these trials, highlighting the pivotal role of advanced techniques like gene therapy and immunotherapy. Furthermore, we will examine the essential contributions of research funding and state-of-the-art lab equipment, which serve as the backbone of this vital scientific endeavor. Join us as we navigate this complex yet incredibly promising domain, understanding how each trial brings us closer to a world free from the scourge of cancer.
Before any treatment enters clinical trials, years of intensive cancer research are conducted in laboratories. This foundational work involves unraveling the intricate mechanisms of cancer at a cellular and molecular level. Scientists leverage advanced molecular biology techniques to identify genetic mutations, abnormal protein expressions, and signaling pathways that drive cancer growth. This deep understanding forms the basis for identifying potential therapeutic targets. The advent of modern biotechnology has revolutionized this phase, providing tools for high-throughput screening, genomic sequencing, and precise manipulation of biological systems, accelerating the pace of discovery and paving the way for novel cancer treatment approaches.
The journey of a new cancer treatment through clinical trials is a multi-stage process, each phase designed to answer specific questions about safety and efficacy:
In Phase I, a small group of patients (typically 20-80) receives the new treatment for the first time. The primary goal is to determine the safest dose, identify potential side effects, and understand how the drug is metabolized in the body. These trials are critical for establishing a safe starting point for further investigation. Patients often have advanced cancer and have exhausted other treatment options.
Phase II trials involve a larger group of patients (typically 100-300) with a specific type of cancer. The main objective is to assess the treatment's effectiveness against the cancer and to continue monitoring for side effects. If the treatment shows promising results and manageable side effects, it progresses to Phase III.
This is the largest and most crucial phase, involving hundreds to thousands of patients. The new treatment is compared against the current standard of care or a placebo. Phase III trials aim to confirm the treatment's effectiveness, monitor side effects over a longer period, and collect information that will allow the treatment to be used safely.
Even after a drug is approved and marketed, Phase IV trials continue to monitor its long-term effects, identify rare side effects, and explore new uses or populations. This ongoing surveillance ensures the continued safety and optimal use of the therapy in the real world.
The cutting edge of cancer therapy is increasingly defined by personalized and targeted approaches, with gene therapy and immunotherapy leading the charge. Gene therapy in cancer research involves introducing, removing, or modifying genetic material in a patient's cells to fight the disease. This could mean inserting genes that make cancer cells more susceptible to treatment, or genes that enhance the body's immune response. These complex interventions are rigorously tested in clinical trials to ensure their precision and safety.
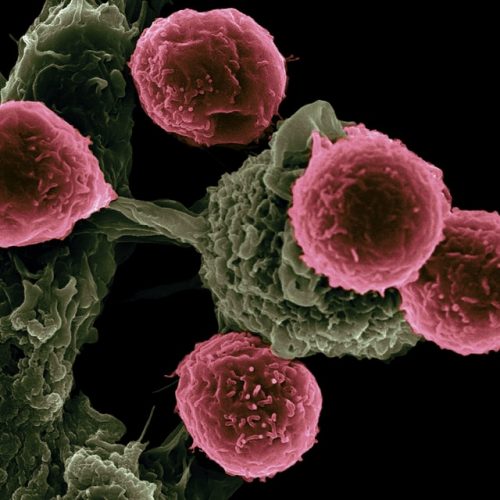
Similarly, immunotherapy harnesses the power of the patient's own immune system to recognize and destroy cancer cells. This can involve checkpoint inhibitors that release the brakes on immune cells, or CAR T-cell therapy where a patient's T-cells are genetically engineered to target cancer. The development of these sophisticated therapies relies heavily on advanced biotechnology and extensive clinical trials, pushing the boundaries of what's possible in oncology.
The path from initial scientific insight to a new approved drug is long and arduous, with drug discovery being the initial critical step. This involves identifying potential therapeutic compounds, often through high-throughput screening of vast chemical libraries or rational design based on molecular targets. Once a promising compound is identified, it undergoes extensive preclinical testing in cell cultures and animal models to assess its safety and efficacy before it can even be considered for human clinical trials. This entire process is a testament to the collaborative efforts across academia, industry, and governmental bodies, all working towards the common goal of advancing cancer treatment.
Behind every successful clinical trial and every breakthrough in cancer research are two indispensable elements: robust research funding and cutting-edge lab equipment. Conducting clinical trials is incredibly expensive, covering everything from patient recruitment and monitoring to data analysis and regulatory submissions. Government grants, philanthropic donations, and private investments are crucial for sustaining this costly endeavor. Similarly, advanced lab equipment – from genomic sequencers and mass spectrometers to sophisticated imaging systems and cell culture facilities – provides the necessary infrastructure for both foundational research and the precise execution of trials. Without these resources, the pace of innovation in biotechnology and molecular biology would slow significantly, delaying the arrival of new treatments for patients.
Patients who participate in clinical trials are true pioneers, contributing invaluable data that benefits not only themselves but also future generations. Their willingness to undergo experimental treatments, often with uncertain outcomes, accelerates the pace of cancer research. Ethical considerations and patient safety are paramount throughout the trial process, with strict protocols and oversight by institutional review boards. Informed consent ensures that participants fully understand the risks and potential benefits. The partnership between researchers and patients is fundamental to the success of clinical trials in cancer research, embodying a shared commitment to overcoming the disease.
Despite significant advancements, clinical trials face challenges, including patient recruitment, the complexity of trial design for personalized medicine, and the high attrition rate of promising compounds. However, the future of cancer research is bright, driven by ongoing innovations in biotechnology and molecular biology. The integration of artificial intelligence and big data analytics is poised to streamline trial design and patient selection. Furthermore, the focus on combination therapies, liquid biopsies, and novel drug delivery systems promises to enhance the efficacy and reduce the toxicity of future cancer therapy. The continuous evolution of Deep Science Workshops and Deep Science Implementation methodologies will further empower researchers to tackle these challenges and accelerate the development of transformative treatments.